We are undergoing a website renovation this summer and can’t wait to show you our new home in the fall. Until we have our full website up, here is the most frequently requested information.
Palliative & Supportive Care of Nantucket (PASCON) is a specialized health care program dedicated to providing excellent physical, psychological, social, and spiritual care for persons with serious illness and their families.
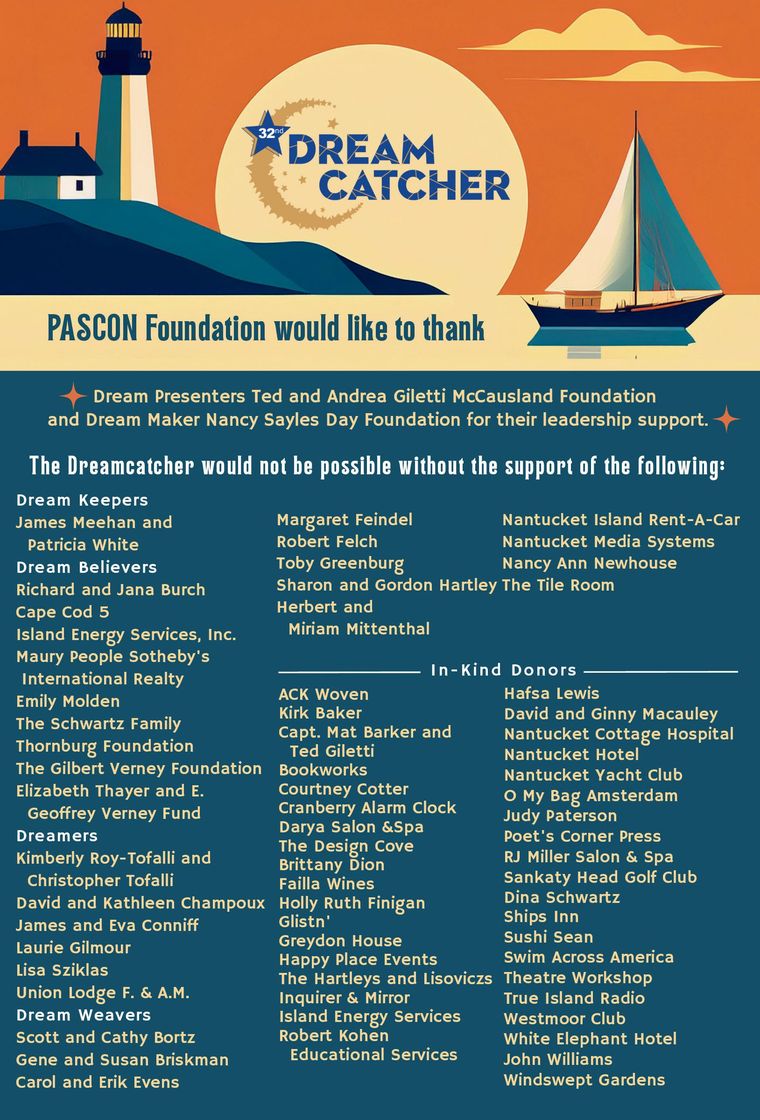
Palliative & Supportive Care of Nantucket Foundation is dedicated to funding all of PASCON’s programs and services so that they may be provided free to the community without insurance reimbursement and to educating the community and raising awareness about palliative and supportive care issues.
The PASCON Department is located in the Nantucket Cottage Hospital.
Call (508) 825-8325 to speak with our staff about our services.
If you are looking for assistance with making a gift, please get in touch with the Foundation at info@pascon.org.
THE MARLA CEELY LAMB CANCER TRAVEL FUND
This dedicated fund for Nantucket residents provides reimbursement for patients’ off-island cancer care and treatment.
Marla, a Nantucket native, conceived of the fund during her personal experience with off-island travel for cancer treatment. This is her legacy.
This fund is solely supported by her family and the generous contributions of the Nantucket community.
To receive assistance or contribute to the Marla Ceely Lamb Fund please contact 508-825-8325.

Swim Across America – Nantucket
Saturday, July 26th
Since 2013, Swim Across America - Nantucket has raised over $5.5 million in support of cancer care on island. Palliative and Supportive Care of Nantucket is a proud and grateful beneficiary of a portion of these funds. Whether you are a veteran swimmer or you're looking to do your first open water swim, we welcome you to help us "Make Waves to Fight Cancer."
Learn more about this event and sign up to swim or volunteer here.